News Story
BIOE Capstone 2017: Projects Focus on Pediatric Care, Physical Therapy, Pulmonary Tumors, and More

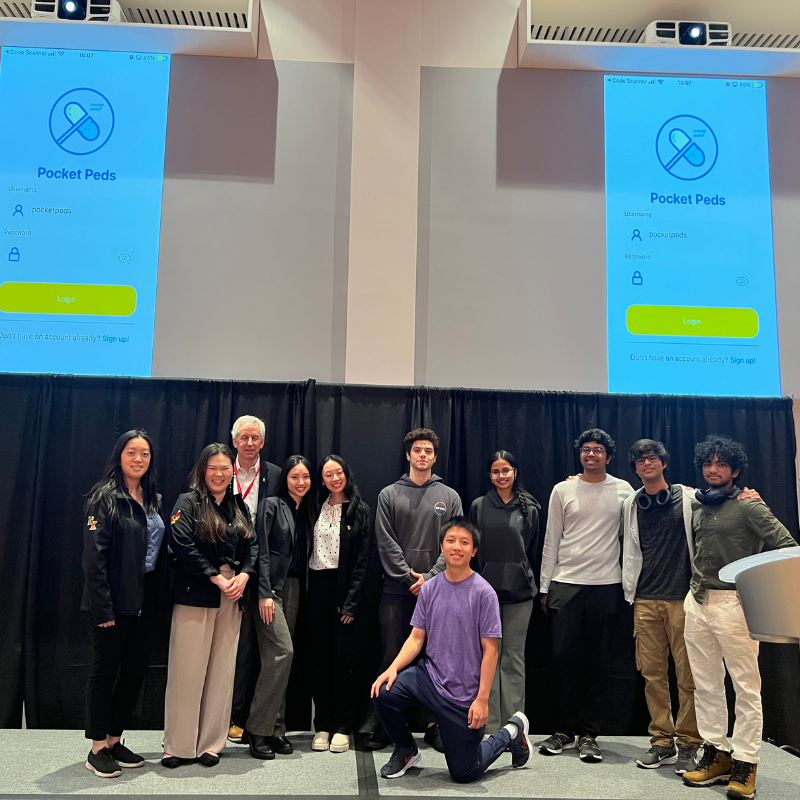
Members of the BIOE class of 2017 with their mentors, BIOE faculty, and Capstone judges.
Showcasing the many ways bioengineers are working to improve human health, the Fischell Department of Bioengineering (BIOE) 2017 Senior Capstone class exhibited a total of 21 novel concepts during the Capstone II finale on May 10, 2017. Photos from this year's event are available online.
Projects ranged from a light-shielding device for neonatal incubators and dissolvable strips to treat allergic reactions. to phototherapy treatment for jaundice in premature infants and a transesophageal blood-cooling device to reduce ischemic brain injury.
The 2017 Capstone Design Competition marked the biggest yet, as 102 students pitched their products to a panel of esteemed judges, as well as to BIOE faculty and fellow students. Created and sponsored by Mrs. Susan Fischell, wife of A. James Clark School benefactor Dr. Robert E. Fischell, the Capstone Design Competition has been a marquee event, capping off the end of the academic year.
This year's panel of judges featured:
- Dr. Anant Agrawal, Food and Drug Administration
- Dr. Kevin Cleary, Children's National Health System
- Dr. Martha Connolly, (Past Director) Maryland Technology Enterprise Institute Baltimore
- Dr. Gregg Duncan, Fischell Department of Bioengineering
- Dr. Ryan Sochol, Department of Mechanical Engineering, Bioinspired Advanced Manufacturing Laboratory
- Dr. Martha Wang, Fischell Department of Bioengineering
- The Fischell Department of Bioengineering Advisory Board
- University of Maryland, Baltimore collaborators
- The Bioengineering Graduate Student Society
Noah Bar-Shain, Leila Ettehadieh, Danielle Rossi, Deena Rubin, Shannon Schreiner

Over 300,000 cardiac arrests occur annually with a patient survival rate of only 10-20%. In addition to this low survival rate, one-third of cardiac arrest survivors display brain damage due to reperfusion injury, which can lead to brain death. Since the 1960s, hypothermia has been used for brain protection in cardiac surgeries during periods of low blood flow to the brain. For every 1 degree Celsius drop in a patient’s body temperature, cerebral metabolic rate decreases by 6%. A current strategy to improve neurological outcomes after cardiac arrest is to cool the brain, in hospital, after the cardiac arrest occurs. However, cooling the brain as soon as first responder treatment begins would be more effective in improving neurological outcomes, as metabolic demand would be reduced at the onset as well as during the time of reperfusion. As the ascending aorta, and aortic arch, are directly behind the esophagus, cooling the esophageal tissue was proposed as a strategy to cool the blood being carried to the brain. In order to accomplish this goal, a novel, controlled, cerebral cooling device prototype, which can be placed down the esophagus during cardiac arrest, was designed and developed. Criteria for this device included: weight, portability, ease of use, disposability, and which could be deployed outside of the hospital by military personnel and first responders, or inside of the hospital by emergency room doctors and nurses. An anatomical model using flesh, heart, and brain analogs was created and a prototype tested. The prototype consisted of a central silicone tube which lent structural stability to the device and would enable insertion into a patient’s esophagus. Cooling media was introduced via a pump, connected an entry tube, which circulated cooling media through a cooling balloon, and returned the media to a cooling repository via exit tube. This design maximized the area of surface contact between the esophagus and balloon. The greatest extent of brain cooling was achieved by the device constructed with a polyisoprene balloon, in conjunction with circulated water, cooled by ammonium nitrate instant cold packs. This prototype demonstrated the feasibility of utilizing esophageal cooling, via liquid filled balloon, as a novel cerebral cooling methodology.
Team 2: PAPRS: Proximity-Activated Patient Restraint System to Prevent Patient Dislodgement of Critical Support Devices
Adam G. Berger, Hye (Grace) Chun, Ashlyn M. Lee, Casey G. Lim, Justin K. Shin
Advisors: Dr. Jeffrey Hasday (University of Maryland School of Medicine), and Dr. Steven Jay (Assistant Professor, BIOE)
Physical or pharmacologic restraints are commonly used following surgery, trauma, or in patients with critical medical illness to prevent them from removing critical medical devices, such as IVs, urinary catheters, or endotracheal tubes. Altered mental states related to the underlying condition, medications, or even waking from sleep, may increase likelihood of inadvertent device removal. Current methods of physical restraint are both easy to evade and overly constraining. If patients evade the restraints, they can remove critical medical devices, potentially causing harm to themselves and often requiring additional resources. Immobilization due to fixed restraints can increase risk of pressure ulcers, aspiration, deconditioning, and delirium, which prolongs the hospital stay. Team 2's solution to the issues with current physical restraints is the Proximity-activated Patient Restraint System (PAPRS). This system allows movement ad libitum, but locks automatically if it senses that the patient’s hands are within a predetermined range of a critical medical device. A webcam provides motion tracking of the patient’s hands relative to their critical devices, all of which are tagged with special stickers recognized by the motion tracking algorithm. A locking mechanism similar to that in a seatbelt can be actuated with a servo to lock the restraints in response to a proximity signal. The system has facile integration with current non-adaptive physical restraints and easily attaches to the side of the bed. Thus, PAPRS is a restraint system that allows unrestrained movement but prevents removal of medical devices by patients. PAPRS may increase safety, improve patient outcomes and satisfaction, and conserve resources, reducing the costs of medical treatment.
Team 3: Dynamic Neonatal Ventilator Tubing Support Device
Billy Beattie, Madison Lawhorn, Steve Madaras, Peter Simone, Shira Winston
Advisors: Dr. Rose Viscardi and Dr. Priya Sundararajan (University of Maryland School of Medicine); Dr. Lester Schultheis (BIOE, Robert E. Fischell Institute for Biomedical Devices)
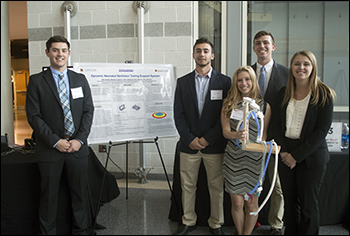
The constant care and monitoring required for premature babies held in intensive care presents opportunities for various innovations and improvements of current technologies within the Neonatal Intensive Care Units (NICU’s). The chosen project aims to improve the support system for ventilator tubing. With the current device used to support the tubing, a portion of the ventilator tubing still presses down on the babies’ faces, which could potentially result in facial deformations and lead to corrective surgeries in the future. The main goal of Team 3's device is to create a dynamic support system that will move with the neonate in order to reduce the risk of extubation and eliminate the need for nurses’ to constantly adjust the system. Additionally, the team has incorporated an emergency release component so that the device can be quickly removed if a situation arises that requires full access to the patient. Currently, their prototype was manufactured with 3D printed PLA components, steel joints, and wooden supports. The intention was to use materials that were inexpensive and could easily be altered in order to aid prototype development. In the future, the goal is to manufacture the device entirely out of acrylic or polycarbonate due to the fact that it is radiolucent, translucent, lightweight, and inexpensive. The device was tested in the UMMC NICU with in the GE Omnibed Giraffe incubator with an intubation mannequin. Suggestions for future developments were made, by respiratory specialists, clinicians, and nurses, including incorporating a single center support, unique and detachable clips for various types of tubing, and the ability to adjust the height so that the device could be implemented in the NICU and PICU (Pediatric Intensive Care Unit). These suggestions would be taken into account in future variations of the prototype. Overall, the need for an improved ventilator tubing support device is crucial for the healthy development of neonates worldwide.
Team 4: Forced-Air Warming Blanket to Combat Perioperative Hypothermia in Infants and Children
Michael Burgan, Megan Dang, Oluwatobi Fagbohun, Angelina Nou, Devayani Srinivasan
Advisors: Dr. Angela Jones (BIOE), Dr. Adnan Bhutta (University of Maryland School of Medicine)
Perioperative hypothermia occurs when a patient’s core temperature drops below 36°C due to anesthesia-induced loss of thermoregulatory function. It can result in problems such as acidosis, coagulopathy, increased susceptibility to infection, and myocardial complications. Infants and neonates are more likely to experience perioperative hypothermia due to their smaller weight to surface area ratio. Currently, the gold standard for perioperative warming is the Bair Hugger, a forced air warming blanket. We aim to make an innovative underbody warming blanket that is reusable and more effective and efficient than the Bair Hugger. We identified two primary focuses to meet this objective. The first was to insulate sides of the blanket that are not in contact with the patient in order to make the warming more effective. To work on this component, we generated models in COMSOL to study how the heat distributions change. The second component was to develop an automated system that takes temperature input from the patient to control the pump and heating unit. For this, we built a prototype system and collected data for specific conditions. Future work will be implemented in order to model how certain insulations will affect the heat dissipation of the blanket. Additionally, different ranges of pumps and heat sources will need to be considered in order to modulate for either high air force or low heat output.
Team 5: AgNovos Healthcare: Advanced Orthopedic Surgical Instrumentation and Delivery System
Shawn Ulmer, Miguel Flores, Van Hoang, Ronelle Bautista, Jovy Batong
Advisors: Dr. Ian White (Associate Professor, BIOE), and Dr. Jonathan Shaul (AgNovos Healthcare)
Osteoporosis is a bone condition that affects over 200 million women worldwide, but the only current treatment is pharmaceutical drugs that can take up to 18 months to reach effectiveness. Because of this, AgNovos has developed a minimally invasive surgical kit to treat osteoporosis in hips. Team 5's project goal was simple: take the already successful kit and improve upon it. Although straightforward, they began the iterative design process by brainstorming ideas based off of feedback from a usability report conducted by Agnovos and several surgeons. Group members wrote proposals for each idea and from there they ranked their ideas with a rubric that listed their most important criteria weighted highest. After choosing to redesign the suction-irrigator, the group went to work designing the new component in 3-D software and after multiple 3-D printing iterations, they came up with the working prototype displayed at Capstone. For the future, the team would like to replace the 3-D printed plastic with a smoother plastic, such as PVC, and scale down the dimensions to closer resemble those of the original piece.
Team 6: Resuscitation Sensors to Enable the First Breath of Life
Kirstie Coombs, Tyler Hao, Jillian Ryan, Matt Schelin, Janna Wisniewski
Advisors: Steven M. Falk (General Electric Healthcare), Karen Starr (BC-NNP), Dr. Edward Eisenstein (Professor, BIOE)
Of the 136 million infants born annually, approximately 10 million require assistance initiating and sustaining their first breaths. Clinicians must perform neonatal resuscitation procedures accurately in order to provide the correct oxygen concentrations and inspiratory pressures. Clinicians obtain feedback through observation of the rise and fall of an infant's abdomen and through oxygen saturation data obtained by a pulse oximeter, but these methods can be subjective, inaccurate, and error-prone. Errors in resuscitation may lead to developmental complications or death. Proper resuscitation requires understanding the end-tidal carbon dioxide (EtCO2) levels, as well as the flow rate of the breath, which can be integrated to calculate tidal volume. The goal of this project is to create an adaptor to be used with GE Healthcare’s Giraffe Stand-alone Infant T-Piece Resuscitation System. This adaptor must contain a CO2 sensor that can accurately measure the EtCO2 and a flow sensor that can be used to calculate the tidal volume. Also, it is important that the adaptor is either low cost so it can be disposable, or easily sterilized so that it can be reused. The team developed the prototype by selecting and testing the sensors, and continuously redesigning the adaptor to fit the size specifications of the current system. The prototyped adaptor contains a NDIR CO2 sensor (CO2 Meter) that sits close to the mask and a differential pressure flow sensor (Sensirion) that is located within the air stream. Both sensors are able to be autoclaved and small enough to be integrated into the resuscitation system. The team tested these sensors in the presence of 4% CO2 gas and at a range of flow rates that simulated neonatal breathing. The sensors displayed accurate and precise readings. This prototype achieves the goals set by the team and would successfully give clinicians greater insight into physiological events occurring during the resuscitation procedure.
Team 7: The Bilimattress - A Phototherapy Treatment for Jaundice in Premature Infants
Andrew Cheng, Marlena Hill, Oren Lagziel, Jonathan Lin, Michael Tobin
Advisors: Dr. Rose Viscardi and Dr. Jocelyn Leung (University of Maryland School of Medicine), Dr. Helim Aranda-Espinoza (Associate Professor, BIOE)
2ND PLACE

Elevated bilirubin levels, clinically termed jaundice, is a common condition which affects 60% of newborn babies as well as almost 100% of premature babies born before 35-37 weeks. This condition visibly manifests through yellowing of the skin and eye tissue with severe cases resulting in kernicterus or death. Treatments for alleviating bilirubin buildup, such as phototherapy, have significantly reduced the cases of newborn jaundice and prevent permanent damage to a newborn’s health. However, no devices have been specifically developed for treating premature infants, a population which have significantly different characteristics than term babies, including highly sensitive skin and smaller size. Our proposed solution, the BiliMattress, provides effective phototherapy treatment for the prevention of jaundice and kernicterus specifically designed for premature infants. The prototype consists of electronic and material-based components integrated into a functional therapeutic device. Ninety high-power LEDs are used in conjunction with an Arduino microcontroller to modulate the irradiance for treatment while dual material layers provide developmental support and thermal insulation for the BiliMattress. Upon testing, the device produced higher irradiance levels (27-50 μW cm-2 nm-1) than market products while introducing custom moldability without excessive heat generation. These features, coupled with its reusability and low cost to manufacture, permit a viable phototherapy alternative for premature infants. Future work includes testing x-ray compatibility, improving gel clarity, and introducing pressure sensors for more efficient use. The final product will be easily implementable into existing NICUs around the country.
Team 8: Autogenic Drainage Spirometric Training System
Andres Gonzalez, Woojae Koh, Erin Walter, Morgan Walter, Jimmy Zhang
Advisors: Dr. Silvina Matysiak (Assistant Professor, BIOE), Dr. Jean Jeudy (University of Maryland Medical Center)
More than 10 million Americans struggle with respiratory disease, such as cystic fibrosis (CF). To relieve symptoms, various airway clearance techniques are recommended. One relatively new technique, autogenic drainage (AD), is now commonly used by CF patients for symptom mitigation. When used in conjunction with other traditional clearance methods, it can help to significantly reduce discomfort. AD is a breathing pattern designed to draw mucus from the airways by inhaling and exhaling between stages of various lung volumes. The technique is currently taught by respiratory therapists, but has the potential to be learned outside of the clinic with proper guidance. The Autogenic Drainage Spirometric Training System, specifically designed to assist young children, instructs the breathing pattern using an interactive gaming system that cues the user to breathe according to a specified curve. The design features a venturi tube body that creates a pressure drop detected by a differential pressure sensor, which is processed by a Raspberry Pi B+ unit and is displayed on an LCD screen. Improvements to the current device include optimizing its accuracy via noise reduction, increasing its portability, and developing a more captivating game. Clinical testing of the device will also prove its effectiveness in both mucus clearance and teaching AD to children in an innovative manner.
Team 9: Mathematical Model of Cartilage Tissue Scaffolds for Use in Failure Testing and Tissue Regeneration Applications
Tanner MacPhee, Dawei Wu, Lauren Jokl, Michael Amorjay-Ogar, Megan Tobin
Advisors: Dr. Ryan Ortega, Dr. John Fisher (BIOE Professor and Department Chair)
For Team 9's Capstone project, they attempted to add understanding and efficiency to the research-based methods that further the fields of tissue engineering and regenerative medicine. They developed a mathematical model of a cell seeded scaffold for clinical use in tissue regeneration. This model will be used in testing for specific mechanical properties of scaffolds of different physical configurations, with the aim of predicting structural failure. The team's main goal for this project is to provide a method of in-silico testing of scaffolds to help ensure the safety of in-vivo implantation. While the first semester of their Capstone experience was dedicated to idea generation and planning, the second semester saw action and the eventual completion of a functional program.
The degradation portion of their model is based on hydrolysis of biological materials inside the human body. Specifically, they focused on the bulk degradation, which governed the equations and conditions used in the mathematical model. Although biomaterial degradation is complex, it can be oversimplified to simple exponential decay where mass loss is defined by chain scission inside the polymer matrix. After settling on this degradation model, Team 9 then moved onto the mechanical testing of their scaffold. Using a two-dimensional Finite Element Analysis method, they applied loads to a small sample of their structure and looked for returned stresses and strains. Based upon these outputs, their model was able to predict the extent of degradation at which a specific biomaterial scaffold would fail.
One major use for this model is to aid in the treatment of Osteoarthritis through the regeneration of cartilage tissue via tissue scaffolds. Osteoarthritis is the degeneration of joint cartilage and is the most commonly medically treated arthritic condition worldwide. With a mathematical model of cartilage tissue, it would be possible to test the scaffold in silico to ensure the safety and efficacy of in vivo implantation. In vivo testing leads to financial and ethical issues, but with in silico results, the risks would be diminished before implantation.
In the future, the team hopes to implement a more realistic degradation rate by understanding the biochemistry of the scaffold matrix. With regards to the mechanics of their scaffold, the addition of a cyclic analysis in the FEA will allow for a better representation of the repetitive load due to the movement of the legs over an extended period of time. Furthermore, instead of just having a 2D FEA for analyzing the stress and strain for each connection within the scaffold, a more viable tool for providing evidence of safety could be executed by applying an FEA to the entire 3D model.
Team 10: Improvement to Percutaneous Dilation Tracheostomy Device
Conor Bloomer, Paige Chan, Peter Chen, Scott Kivitz, Torrance Wang
Advisors: Dr. Joseph Rabin (University of Maryland Medical Center), Dr. Silvia Muro (Associate Professor, BIOE)
MPOWER AWARD
A tracheostomy is a surgical procedure that involves creating a hole in the trachea and inserting a tube to provide airflow to the lungs and protect the patient’s airway. Commonly used techniques are either a standard open surgical procedure or a percutaneous device, such as the Ciaglia Blue Rhino® percutaneous tracheostomy kit. While the percutaneous approach may offer various advantages including fewer associated complications, current methods require the use of multiple dilators and exchange of these over a guide-wire or bougie. The current procedure is cumbersome and potentially time-consuming and is not approved for airway emergencies. As a result, there are aspects of the available designs that can be improved. Design modifications focused on reducing the number of components in the kit to simplify the procedure. A single component device was designed to incorporate a standard bubble test to assess entry into the airway and needle retraction into the device and guide-wire advancement into the trachea to increase efficiency. A variable diameter dilator was designed to expand a region of the device radially with vertical compression of a plunger under the provider’s control. The goal of this project is to develop a more efficient device that can safely insert a percutaneous airway both electively and emergently avoiding the risks and reducing the resources associated with an open procedure.
Team 11: Addressing Patient-Ventilator Dyssynchrony
Zachary Bolten, Timothy Holzberg, Ben Kaplan, Catherine Panasenkov, Robert Rosen
Advisors: Dr. Nirav Shah and Dr. Laura Ferguson (University of Maryland Medical Center), Dr. Christopher Jewell (Assistant Professor, BIOE)
Mechanical ventilators are used to support the breathing of patients in critical medical conditions with diminished respiratory control. Even though mechanical ventilators are found in all intensive care units (ICUs), current models are unable to detect whether the patient’s breaths are synchronous with those of the ventilator. Ventilators are utilized by 39.5% of ICU patients, and 24% of these patients experience patient-ventilator dyssynchrony. While dyssynchrony does not pose an immediate danger to the patient, it can often lead to numerous long-term complications including diminished gas exchange in the lungs, compromised hemodynamics, increased cardiac output, and hyperinflation of the lungs.
Despite these issues resulting from patient-ventilator dyssynchrony, clinicians have little time to actively search for these irregularities due to the fast-paced environment of the ICU. Team 11 aimed to improve the functionality of current mechanical ventilator systems by developing an algorithm to detect dyssynchrony in ventilator waveforms of flow and pressure data. They specifically set out to detect two common types of dyssynchrony: the presence of unintentional positive end-expiratory pressure (known as auto-PEEP), and the delivery of two consecutive inspirations prior to exhalation (known as double triggering). Additionally, they aimed to design a method for autonomous measurement of a patient’s plateau pressure, a metric used to evaluate a patient’s respiratory system health. Team 11 designed a dyssynchrony detection system in MATLAB to check for characteristic features of double triggering and auto-PEEP in sixty second intervals. An alarm system was incorporated into the circuit to alert clinicians of the presence of patient-ventilator dyssynchrony.
In order to test the efficacy of the algorithm, standard synchronous and dyssynchronous waveforms for both pressure and flow-controlled ventilation were developed using clinical data provided by the University of Maryland Medical Center. These waveforms were displayed using a dynamic graphical user interface (GUI). The system was able to detect auto-PEEP with an accuracy of 75% (n=8) and double triggering with an accuracy of 100% (n=4). In order to autonomously measure plateau pressure, a rotating valve was designed using computer-aided design (CAD) software and manufactured using a 3D printer. The valve allows air from the ventilator to be diverted to the atmosphere by controlling a gate using a position-based servo. MATLAB to Arduino communication was used to rotate the valve at preset intervals. This enables the autonomous performance of an end inspiratory hold, a maneuver that currently requires manual work from clinicians. An air pump and a differential pressure transducer were incorporated to demonstrate the ability of the valve to rotate the gate, measure plateau pressure, and display this pressure on the GUI.
There are many improvements to be made to Team 11's design, including testing the algorithm with real-time patient data, expanding the modes of dyssynchrony detection, improving the valve design for measuring plateau pressure, and incorporating their device into existing ventilation systems. They anticipate that these improvements can be implemented successfully with additional time, effort, and funding. It is their hope that the unique features employed in their device can be implemented into current ventilator systems to reduce workload for medical professionals, minimize health care costs, and improve patient care.
Team 12: Reinventing the Neonatal Phototherapy Eye Shield
Deja Duncan, Allison Dunn, Jillian Holt, Nicole Sabatelli, Brooke Sauter
Advisors: Dr. Rose Viscardi and Dr. Jocelyn Leung (University of Maryland Medical Center), and Dr. Giuliano Scarcelli (Assistant Professor, BIOE)
Premature babies are at risk for hyperbilirubinemia, the buildup of bilirubin in the blood and eventually brain tissues. This condition is typically treated by phototherapy, which involves shining a 390-510 nm light over the infant’s body. However, eye exposure to this light for extended periods of time can cause cell destruction or blindness. The aim of the neonatal multifunctional phototherapy shield is to reduce eye exposure of this intense light during phototherapy. The device allows maximum exposure of the infant’s skin to the light source while protecting the eyes. The overall goal for this design is to facilitate the healthy development of these babies and to ensure practicality for the nursing staff.
The product most commonly used to protect premature patients’ eyes from the phototherapy is a disposable eye mask placed directly over the eyes. This product causes problems with patient treatment due to its tendency to slip off of the eyes and its blockage of all wavelengths of visible light. By refraining from direct contact, the use of an overhead shield minimizes mask displacement due to movement. The design also facilitates an increase in movability of the baby without interfering with the device, and by blocking only the wavelengths of visible light used in phototherapy, encourages the babies to develop natural circadian rhythm.
The shield is made of acrylic that will reduce the transmittance of the phototherapy light while allowing for the transmittance of all other wavelengths of visible light. Other features of the neonatal phototherapy eye shield include adjustability to accommodate different angles of phototherapy lamps and ease of access so that the device can be moved if necessary for the patient’s treatment. Based on testing of the device, it was determined that the shield is successful in blocking the transmission of light wavelengths 390-510nm. The shield also ensures that the light that reaches the eye is below the threshold level for retina damage.
Team 13: Electrochromic Light Shielding Device for Neonatal Incubators
Tomer Zohar, Ben Shafer, Dave Hesley, Elijah Biggs, Scott Ensel
Advisors: Dr. Yang Tao (Professor, BIOE), Steve Falk (GE Healthcare)

In a single year, fifteen million premature and low birth weight babies are born. During the first four weeks of life, 2.7 million of these infants that die due to prematurity, asphyxia, and infection. Neonatal incubators support growth and health by providing an isolated environment that regulates oxygen levels, temperature and humidity. One under-controlled environmental factor is light, which is usually completely shielded using a hood blanket. Studies have shown that cycled light produces significantly higher weight gain and shorter length of hospital stay in neonates. GE Healthcare’s Maternal Infant Care team, a leading provider of neonatal products, tasked Team 13 group with fabricating a surface amendment to the acrylic hood of their Giraffe Incubator Carestation. This amendment must have light-shielding capabilities and allow diurnal light cycling to the infant within the incubator. The team's solution, a Lithium-ion electrochromic device, meets GE Healthcare’s expectations by functioning near 50-90% transparency, using automatic actuation through a control system, and having the capability to withstand industrial cleaning. Team 13's light-shielding device will allow GE Healthcare to integrate the technology onto their current incubator units at low relative cost, decrease neonatal hospital stay, and ultimately decrease infant mortality rates, the student group said.
Team 14: Expandable Cryoablation Device for Pulmonary Tumors
Nadia Alam, Danielle Brown, Jason Colasanti, Meghan Miller, Kevin Reid
Advisors: Dr. Ashutosh Sachdeva (University of Maryland Medical Center), Dr. Ian White (Associate Professor, BIOE)
1ST PLACE

Lung cancer is the most common cancer worldwide and claims the lives of over 1.35 million patients annually. Stage I and II lung cancers are best treated with minimally invasive bronchoscopic surgery. Current surgical devices are efficient for removing exophytic tumors which grow on one side of the airway (Case 1), but are inefficient for removing concentric infiltrating tumors which grow around the entire inner circumference of the airway (Case 2). During removal of Case 2 tumors, the shortcomings of current surgical methods are extensive surgery times upwards of 2 hours, excessive scar tissue formation, and increased likelihood for additional surgeries for stent implantation. Team 14's proposed device employs a cryogen and an expandable metallic mesh to increase tumor-device surface contact area, thereby increasing yield and reducing projected surgery times, as well as reducing scar tissue formation due to cryotheraputic capabilities. In the device design, a 15-mm long cylindrical 18K gold mesh is threaded over a PET angioplasty balloon with bilayer catheter flexible tubing, and inserted through the bronchoscope working channel. Upon contact with the tumor, this mesh is simultaneously expanded and cooled by pumping the cryogen into the balloon. Cycling liquid nitrogen cryogen into the angioplasty balloon expands, cools the mesh to -40 °C, initiates contact by slightly pushing the mesh into tumorous tissue around the airway circumference, and then freezes the mesh-tumor interface, such that when the mesh contracts the frozen tumor is ablated. Proof-of-concept experiments to evaluate the safety and efficacy of the device reinforce the endurance and elasticity of the PET angioplasty balloon while containing liquid nitrogen, the strength of 18K gold to withstand expansion, and ablation by mesh contraction. Mathematical models were also created to determine the rate of heat transfer from the cryogen to the angioplasty balloon, gold mesh, and tumorous tissue. Depth of time-dependent penetration for cooling is modeled to ensure that the mesh does not deliver excessive cooling, to optimize time and patient safety. The accomplished device objectives of reducing surgery time and scarring confer reduced complications and surgical costs for the patient and surgeon.
Team 15: Physical Therapy Modulation Device for Intensive Care Unit (ICU) Patients
Matthew Din, Brian Morris, Courtney Restivo, Daniel Wang, Olivia Webster
Advisors: Dr. Laura Ferguson and Dr. Nirav Shah (University of Maryland Medical Center), and Dr. Ben Shapiro (Professor, BIOE)
Every day of bed rest that a patient endures in the Intensive Care Unit (ICU) lowers muscle strength between 3% to 11%.This leaves ICU survivors with a decreased quality of life due to lasting physical damage after discharge. Rehabilitation strategies need to be prioritized in the ICU patient treatment plan. This would lessen the time that patients spend on bed rest, in an effort to maintain and improve their physical health. However, this goal is difficult due to physical therapists seeing on average 6 patients a day out of a total of 29 ICU patients. A physical therapy (PT) modulation device could serve not only to promote muscle retention but also to allow independent patient improvement outside of the time with the physical therapist. Team 15's prototype, PhysAid, was created as a device to fulfill this clinical need. PhysAid is a flexible arm band integrating an Arduino, batteries, an accelerometer, a muscle sensor with electrodes, and a Bluetooth module. The device records overall movement and measures muscle activity. Data collected by the Arduino is transmitted by Bluetooth, imported to MATLAB, scaled to a point based system, and displayed on the user interface. This gives the patient a real-time score based on the amount of movement accomplished throughout the day. Also displayed is weekly progress to show trends in patient movement, allowing analysis and exercise modification by the physical therapist. Suggested future directions include miniaturizing electrical components for a more compact device and transitioning the user interface to a mobile display. Integrating the device’s data with the ICU’s central data system and expanding the use of PhysAid to both arms and legs are also future goals. This device serves as a supplement to PT in the ICU and promotes improved patient outcomes.
Team 16: Evalve - Radially Expanding Pulmonary Valve
Joshua Kim, Sunghoon Lee, Sunny Lee, Phillip Tran, Jeffrey Yang
Advisors: Dr. Ashutosh Sachdeva (University of Maryland Medical Center), Dr. Keith Herold (Associate Professor, BIOE)
Aspergillosis encompasses a wide variety of pulmonary fungal infections that affects more than 4 million people worldwide, while the chronic, invasive, and allergic forms of aspergillosis cause 600,000 deaths annually worldwide. Current treatments involve the insertion of a balloon catheter into the lung to block off the infected area and administer concentrated dosages of amphotericin B. Although each operation lasts a maximum of 30 minutes, the patient has to return to the operation room several times a week to repeat the procedure to compensate for decreased drug efficacy. In order to lower operation room visits, Team 16 proposed eValve, a radially expanding pulmonary valve that is inserted into the bronchioles of the lower lung to isolate the infection and increase drug administration efficiency. eValve is composed of a nitinol metal framework surrounded by a silicone membrane that the clinician can poke a resealable hole through to insert amphotericin B into the afflicted portion of the lung. In ex vivo testing of the prototypes, eValve was shown to prevent drug fluid leakage inside pig bronchioles with target diameters of approximately 10mm.
Team 17: Epistrips: Epinephrine Delivery via Sublingual Dissolvable Strips
Neel Bhardwaj, Joseph Dawson, Darya Goudarzi Taemeh, Yvette Mann, Kevin Xiong
Advisors: Dr. Jean Jeudy (University of Maryland Medical Center), Dr. Lan Ma (BIOE)
BEST ABSTRACT AWARD

Over 50 million Americans suffer from allergies each year, many of which can cause serious adverse reactions and anaphylaxis, which is life threatening. The EpiPen is currently the most common treatment for anaphylaxis. Recently, the price has gone up 500%, making it harder for people buy. Other factors, such as the needle and injection procedure itself, make the EpiPen a burden on many people. We have developed a sublingual dissolvable epinephrine strip, where the drug will diffuse through the sublingual mucosa and into the bloodstream, thereby eliminating the use of a needle and providing rapid drug delivery. In order to obtain the optimal strip, concentrations of the polymer, pullulan, were tested in a mixture with water. Two plasticizers, glycerin and propylene glycerol, were tested for their overall plasticity, flexibility, and dissolution time. Two different epinephrine concentrations were added to the strips, and dissolution time was monitored in vitro. Comsol was used to model diffusion of the epinephrine through the mucosa. Team 17's results indicate that propylene glycerol is the optimal plasticizer, along with 1g of pullulan. Utilizing 5 mg of epinephrine, or 0.806 mg/cm^2, they found that the dissolution time ranged from 20-40 seconds within 5 trials, with an average time of 29.63 seconds. Eventually, strips will contain human dose requirements, which was calculated to be 40mg of epinephrine. Dissolution time will be tested, along with pharmacokinetic studies in clinical trials to ensure diffusion of the drug.
Team 18: Implementation of Single Dynamic Zeolite-Bed within Oxygen Concentrator for Low Resource Settings
Julie Boylan, Diana Curtis, Pierrot Nsengimana, Lalithasri Ramasubramanian, Paul Wampler
Advisors: Dr. Gregory Payne (Professor, BIOE), Dr. Adnan Bhutta (University of Maryland Medical Center)
ADVISORY BOARD AWARD FOR TRANSLATIONAL DESIGN

Oxygen therapy is an essential treatment for hypoxemia, the condition of having an abnormally low concentration of oxygen in the blood and a symptom of several pulmonary and circulatory diseases, such as pneumonia. Despite its importance in treating hypoxemia, oxygen is nonetheless in low supply in many low resource areas of the world, which is one reason why pneumonia is still the second most prevalent cause of death in children under the age of 5. Oxygen concentrators have been proposed as a solution to this problem, as they produce medical grade O2 from the atmosphere; however, current oxygen concentrators on the market are too expensive, require too much power, and are too complex for most low resource settings. To address these limitations, Team 18 developed a preliminary prototype for a simplified, costeffective oxygen concentrator that requires about 205.4 W of power and costs about $460 to build. The device relies on the use of two cycles of compressed air through a single molecular sieve (zeolite) bed. The cycles are controlled via Arduino powered solenoid valves. This allows for oxygen purity to rise in the system during the cycles (valves opened) and maintain the oxygen at a highly purity in a surge tank while the zeolites are being exposed to air, to depressurize and regenerate (valves closed). Furthermore, the device is kept mechanically and electronically simplistic enough that it would not require a trained medical technician to perform any repair work. The system is most suited for deployment in a clinical setting as a stationary oxygen concentrator.
Team 19: Development of a Sensored Peripheral Venous Catheter that Verifies its Placement in the Vein
Sriramya Ayyagari, Chris Comfort, Gino DeFilippo, Dani Khalilzadeh, Anuj Lagowala
Advisors: Dr. Yu Chen (Associate Professor, BIOE), Dr. Ron Samet (University of Maryland Medical Center)
IV catheters have been used in clinical medicine for more than 60 years, and are integral to the patient care process as they allow for the passage of anesthesia and therapeutics into a patient. However, a misplaced intravenous (IV) catheter can lead to serious complications such as phlebitis and extravasation. As a result, there is a clinical need for a system that can allow for constant monitoring and detection of a peripheral IV catheter. A system was created to monitor the position of a catheter used in intravenous access. This device consisted of a coherence-gated doppler sensor that monitored the speed of blood flow around a fiber in the catheter tip. The sensor data was then analyzed using a Matlab program that determined the type of tissue the needle tip was in. From this information, Team 19 was able to determine the location of a placed IV catheter. Data collection and analysis demonstrated that this system is capable of sensing blood flow within a vein and accurately monitored the location of the catheter tip in real time. Further refinement of this design is needed and a potential alternative sensing modality, dual fiber laser doppler flowmetry which would be used to construct a similar system that could acquire flow data with better resolution and more cost-effective components.
Team 20: Computational Modeling of Cell Delivery through a Catheter
Ki Beom Kim, Andrew Lee, Troy Hagerman
Advisors: Dr. Bill Bentley (Professor, BIOE), Dr. Ryan Ortega (Food and Drug Administration)
Many modern medical treatments involve surgeries to repair and regenerate targeted organs, but with difficulties in operation and inherent dangers. On the other hand, the catheter-based transport of therapeutic cells for regenerative medicine is a promising field due to its minimally invasive nature. The catheter-based approach involves delivering cells through a tubing of specific composition and geometry through natural cavities in the body. For this method to be successful, the viability of cells traveling through the system is an important factor. Many factors can affect the viability of the cells in the catheter, and in this project the relationship between shear stress and cell viability is examined. Cell viability is impacted by the shear stress applied during flow through the catheter tubing, especially at the walls of the catheter where the cells experience a maximum shearing stress. In order for device using these physics to be approved, it must pass validation steps and clinical testing for safety. However, the current standard practice for the validation of relevant devices includes a large amount of in vivo and in vitro experimentation, and these tests can be very time consuming as well as prohibitively expensive. In this project, a computational model in COMSOL was built to highlight the best and worst-case scenarios which can be tested for validation. By narrowing the parameters of these tests, a bulk of time and resources for testing catheter configurations can be saved. The model was built using training data that related four catheter builds with various initial flow rates to their cell viability after flowing through the catheter. This model was then tested on a second data set that related shear stress to cell viability and was found to have some general tendencies in common, but did not wholly capture all of the parameters of the system. The estimate on the optimal flow rate to be used was not the local minimum, although it was a value consistent with the data and one of the lower values of cell viability loss seen. It was found that the initial cell viability before loading must correlate with the expected cell viability. Future approaches to modeling cell flow through a tube should focus on incorporation of modeling the transport of the cells through the catheter and looking into modeling both shear rate as well as the initial cell viability.
Team 21: Measuring Membrane Permeabilities for BD Bactec Blood Diagnostic System
Chad Artman, Sean Barker, Nathanael Bowen, Jordan Gorsuch
Advisors: Dr. Peter Kofinas (Professor, BIOE), Edward Carrese (Becton Dickinson)
STUDENTS' CHOICE AWARD
Becton Dickinson (BD) is a world leader in medical devices and lab equipment. Our team has been working with BD’s diagnostics team to provide supporting data for an improvement in their BACTEC product line. The BACTEC system is an automated blood diagnostics system that detects blood infections. The system works by collecting a blood sample from a patient and placing it in a liquid media contained in a vial. The vial is then incubated within the system and is automatically flagged if pathogens are detected. While the current model is successful in the field, there is a desire to bring down the time-to-detection, as this will further minimize patient risk and make the system more cost efficient. To do this, BD seeks to transition from a fluorescence-based detection method monitoring the liquid media, to a more direct method involving measurement of the accumulating CO2 in the vial. This requires a second compartment where the CO2 can collect. Because the vial is agitated as part of the device operation, there is a need for a semi-permeable membrane that allows the passage of CO2 into the second compartment, while blocking the passage of the liquid media. The goal of this project was to develop an experimental protocol and apparatus to test membrane permeability empirically. The empirical data was then used to generate models to predict diffusion rates when membrane parameters are changed. Multiple membrane material candidates were selected and tested, and their characterization data will be analyzed and compiled into a report to BD, which will allow them to make an informed decision on a material for the device.
Published May 17, 2017